Not a BFZ community? Learn about the Built for Zero movement to end homelessness
User Guide for COVID-19 Cost Estimator Tool
May 7, 2020Accessing the tool
The web-based tool is now available here. For Built for Zero communities wanting a more detailed version of the tool, you can access your spreadsheet version of it by logging into your community’s Change Package. Reach out to bfzdatasupport@community.solutions if you need help logging in.
Purpose
The tool can be used to estimate the need and cost for the following interventions:
1. Providing quarantine and isolation (Q&I) units to adults experiencing homelessness who are screened as symptomatic for COVID-19 or have tested positive for COVID-19 (*see footnote on population);
2. Providing permanent housing placements to members of high-risk communities experiencing homelessness, to shield them from infection. Estimated for:
- Individuals experiencing homelessness who are over the age of 50 (**see footnote on age);
- Individuals experiencing chronic homelessness.
Snapshot
The tool also allows you to report and add up your existing funding streams tagged to these interventions and quickly assess the gap between what you have and what you’ll need. This gap analysis is intended to facilitate your community’s conversations with funding partners around right-sized financial support and help you and your teams save lives.
You can adjust a range of parameters in the tool, including
- population size
- infection prevalence
- cost per bed, and
- length of intervention.
We recognize that these are far from the only relevant variables and acknowledge that this tool is far from perfect (see caveats below). We hope it will nonetheless be helpful in determining the order of magnitude of your community’s needs.
Watch a tutorial
How to use this tool
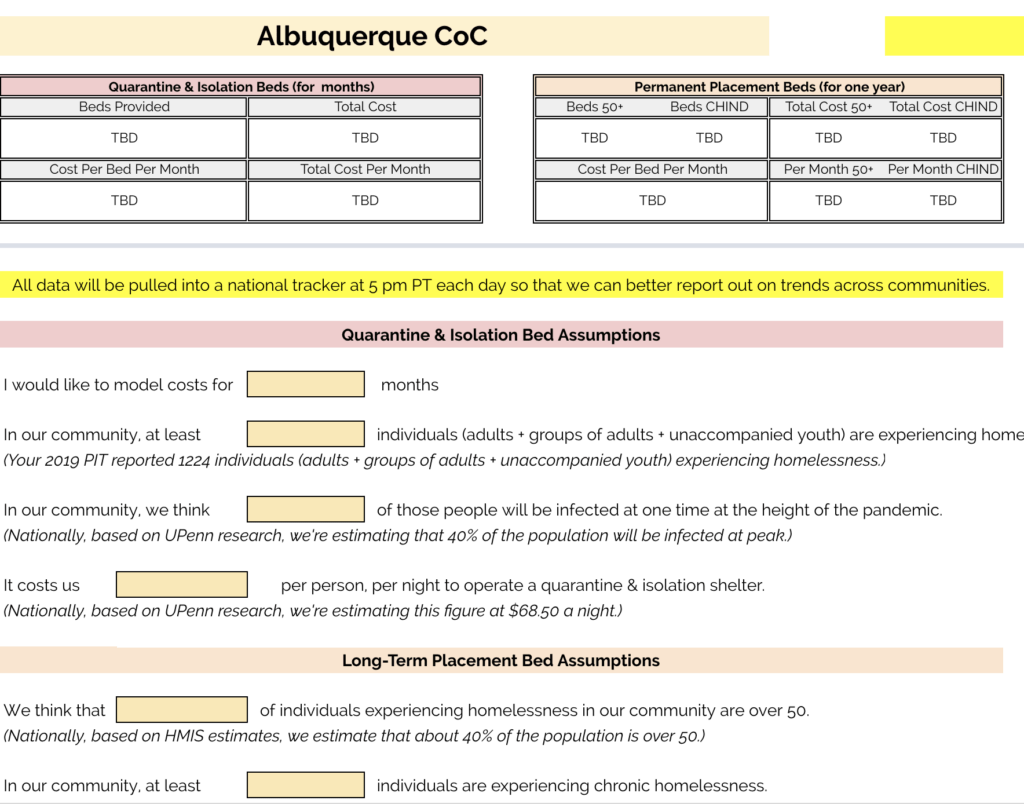
When you begin entering data, the top portion of the sheet will appear blank:

You do not need to enter data directly into these cells. They will automatically update as you enter data, beginning below the horizontal grey line directly below the image above.
Once you enter all your data (descriptions below), the image will update with estimates informed by your assumptions and data. You can update these assumptions at any time.
Continue by entering data into each of the fields below that horizontal grey line.
- Please note that all data in your sheet is accessible to our team, and will be pulled into a national tracker at 5 pm PT each day so that we can better understand and report out on trends across our communities. We are aggregating the data in order to understand national and local trends. We will use this information to continually refine our support to communities, advocate nationally and enlist support from our network of partners.
Quarantine & Isolation Bed Assumptions
1. Months to Model

Enter the number of months for which you’d like to model costs. Most communities do not expect to shelter individuals in quarantine & isolation beds for a full year, for example, as the peak of the pandemic is expected to come within 1-3 months (consider using this tool to estimate the length you’d like to model). If you do want to estimate costs for a full year, just enter 12.
2. Number of Individuals Experiencing Homelessness
Enter the total number of individuals experiencing homelessness in your community (***see footnote on communities). The number of individuals you reported in your January 2019 PIT count is given directly below the data entry field for reference, but because that data is now more than a year out of date you may decide to update this figure with more accurate data from your community.
- Please note again that the PIT figure reported is for individuals experiencing homelessness in your community (single adults, unaccompanied youth, and people in multiple-adult or multiple-child households). This includes both sheltered and unsheltered individuals. If you would like to estimate costs for all people, including people in families, simply enter the higher figure in this field.
3. Maximum Share of Population Infected At Once
Enter your best estimate of the maximum share of your overall population of individuals experiencing homelessness who you believe will be infected at one time during the height of the pandemic. In other words, even if you believe that 85% of the population will be infected over the course of the pandemic, the number you need to know to estimate the number of quarantine beds is the maximum share infected at one time.
- Based on epidemiological estimates by Dennis Culhane and his co-authors, published on March 25th, we’ve estimated this figure at about 40 percent nationally. The percentage is likely to vary significantly by community depending on the degree to which social distancing and other public health measures have already been put in place, but we recognize that will be hard for you to predict.
- We recommend consulting with local public health authorities to estimate this figure for your community, and defaulting to Culhane’s estimates if you can’t.
4. Cost Per Night, Per Person, of Providing Quarantine & Isolation Beds
Estimate the cost of one night of isolated shelter for one person in your community. Culhane and his co-authors, in the paper cited above, estimate a cost of $68.50 per person per night, which works out to $25,000 per person per year and likely reflects a negotiated rate for a hotel or motel.
- These figures are likely to vary significantly by community and our current estimates may well be lower than those operating in your context.
- Please also consider the possibility of using isolated wards within school gyms or sports stadia as you estimate costs, and be sure to include costs of bed, staffing, and other associated expenses.
Long-Term Placement Bed Assumptions
Most of the assumptions from Quarantine & Isolation carry over. A few more are needed:
1. Share of Population Over The Age of 50
You may wish to provide long-term, preventative placements to homeless individuals in your community at high risk of complications from COVID-19, including those over the age of 50. In this field, enter the share of the population of people experiencing homelessness you are estimating for that is over the age of 50. This will help determine the universe you will consider providing long-term placement to, so the model is quite sensitive to this assumption. Our national estimates suggest this figure is close to 40% for major cities, but your data will of course be more accurate for your community.
- Remember to estimate only for the population of individuals experiencing homelessness, and not for all people (including families with children, who will of course have many people under the age of 18).
2. Number of Chronically Homeless Individuals
You may also wish to estimate long-term placement costs for individuals experiencing chronic homelessness, rather than for all individuals 50+ (the tool will report data on both, provided you enter data in both fields). In this field, enter the total number of individuals experiencing chronic homelessness in your community. The number of these individuals you reported in your January 2019 PIT is given below the data entry field for reference, but because that data is out of date you may wish to update this figure with more accurate data from your community (in particular, from your quality by-name list if you have one!).
3. Cost of Permanent Housing Placement
Enter the annual cost of placing someone in supportive housing. We estimate these costs at $12,800 annually, based on National Alliance to End Homelessness (NAEH) analysis, but we expect this number to vary significantly depending on the vulnerability of the population you intend to house and the nuances of your specific market.
Existing Beds Worksheet
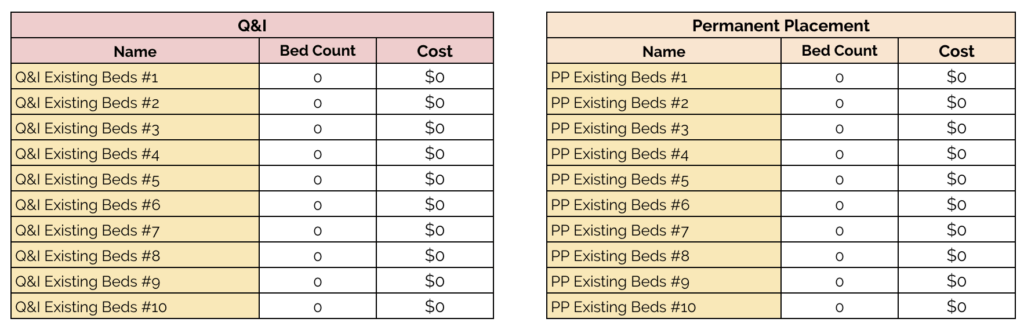
You may have already secured some of the beds you need. Use this section to enter the existing beds in each category which you have already secured and allocated funding for, and at what cost (remember that the tool will assume these costs are over the period of months you’re estimating for, so adjust accordingly if this is not the case). The beds you record here will automatically be accounted for at the real cost you paid for them and not at the per-person projected costs you’ve given elsewhere.
- For example, if you use the tool to project a total need for 500 beds (and assume you’ll pay $68.50 for any beds you haven’t already secured), and you have already secured 100 beds at a local high school at $25 a night, the tool will calculate your total projected cost as 400 beds at $68.50 a night + 100 beds at $25 a night. We want this to be as accurate as we can!
Existing Funding Worksheet
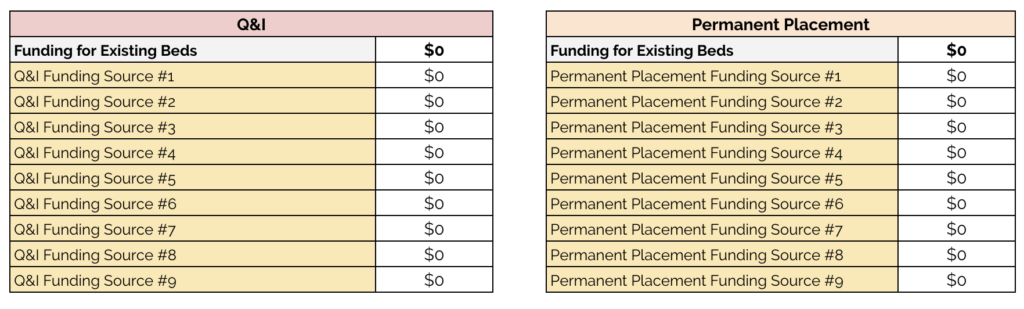
We hope this tool will be used to estimate the additional funding you may need to secure to provide all the beds you need. Use this section to enter the existing funding streams you have already secured to support either Q&I beds or Permanent Placement beds, so that you can assess how much additional money you need to seek after accounting for those funds.
Enter the name of the funding stream you’ve already secured in the left column and the amount in the right column. If funding can be applied to both categories, enter it in both columns as you make your estimates, but remember to leave it in only one once you’re finished, to avoid double-counting. The costs you’ve already entered in the Existing Beds worksheet are accounted for in the Funding for Existing Beds row, as those are funds you’ve already secured and allocated for a particular purpose (and thus don’t need to go after).
Quality Check
Learn more about our process for vetting information.
Scope
Authority
Novelty
Qualifications
Open Questions
Caveats & Qualifications
A caveat to the caveats: This list of qualifications may not be complete and certainly does not represent being a full list of this tool’s limitations. In this fast-moving crisis, we have prioritized distributing a tool that helps communities make some basic assumptions, while still recognizing (as mentioned above) that these are far from the only relevant variables. Again, we hope that the tool will nonetheless be helpful in determining the order of magnitude of your community’s needs, and welcome your feedback. Some specific notes:
- The tool does not account for individuals who fall into both Q&I and permanent placement settings. You should therefore avoid summing the two values to return a total cost, as permanently placing individuals may reduce the need for quarantine & isolation beds. We recommend that you adjust the total number of individuals under consideration to account for some overlap in these populations should you choose to implement both interventions simultaneously.
- The tool does not account for scale-up and scale-down of Q&I beds. In other words, it assumes that you’ll be funding beds at maximum capacity for the entire period under consideration. This will almost certainly not be true in your community, as you will only need to fund the maximum capacity for a limited period of time. In order to account for this, we recommend modeling costs month-to-month by adjusting the number of months you’re projecting costs for.
- This tool does not recommend the use of PIT data in lieu of more recent or more accurate data. If you have better data, use it. PIT count data is provided below each field only to provide a rough estimate for your use and quick-startup, not to suggest that better data is not available — in many cases, we know that it is.
- This tool does not recommend particular public health interventions. Although we model costs for three interventions, we recognize that public health guidance is still evolving and that other interventions may be more appropriate for your community’s needs. We also know that there may be better ways of documenting vulnerability than estimating the number of chronically homeless individuals or the share of the population 50+. If you have better numbers, by all means use them.
- The tool assumes that 100% of funding reported will go to these interventions. We recognize that certain funding streams may be spread out over a number of programs and cost centers, and understand that this may mean that unallocated funding cannot entirely go to these interventions. We recommend that you report the amount of funding that you believe can be targeted to these interventions.
Footnotes
* Footnote on Population
- Because nine in ten families experiencing homelessness are sheltered, and most of those people are sheltered in isolated units, all estimates using this tool are for the population of individuals experiencing homelessness, as defined by the 2019 AHAR, Part 1. This group, which includes about 65% of all people experiencing homelessness and the vast majority of those who are unsheltered or in congregate shelters, includes single adults, unaccompanied youth, and people in multiple-adult or multiple-child households. Communities wishing to estimate costs for their entire population experiencing homelessness, including people in families, can do so by adjusting their estimates of the total population accordingly.
** Footnote on age
- Dennis Culhane and co-authors, in a paper published March 25th, estimate members of this population to be in the high-risk group, despite CDC guidance noting high risks for those age 65 and older, due to “the accelerated physical decline and mental weathering that frequently results from repeat exposure to harsh elements.” Following that guidance, we attempt to identify the population of people over age 50, rather than over age 65, here as well.
*** Footnote on Communities
- The unit of analysis for this tool is the CoC (because it draws on PIT data), so communities that operate over only a portion of a CoC should adjust their figures to capture only the share of the total in their community.
Feedback
Your feedback on this guide and this tool is welcome. Email comments to your Improvement Advisor/Transformer.
This tool was developed by
Community Solutions in partnership with Kaiser Permanente.