Not a BFZ community? Learn about the Built for Zero movement to end homelessness
Personal protective equipment and staff safety in isolation and quarantine settings
April 21, 2020Given that the clinical picture of COVID-19 is ever changing, and that the information about response is changing in turn, Built for Zero anticipates there might be new information on this topic. Please keep an eye out for updated information as new resources emerge.
Last Updated April 21, 2020
Where should different groups of people experiencing homelessness (people under investigation, COVID-19 positive, COVID-19 negative) be placed?
The State of California and the UCSF Benioff Center recommends the following groupings of sites for people experiencing homelessness:
For persons under investigation:
- Quarantine hotel/motel/trailer or other place where individuals can be isolated from others during investigation. (Quarantine Hotel).
- Alternative care settings: group facilities (i.e. shelters) separated from presumed COVID-19 negative individuals and staffed by health care professionals where individuals who are under investigation can receive health care and assessments to see if they require higher level of care (i.e. transfer to emergency department or inpatient).
For people who are COVID-19 positive:
- Alternative care settings: group facilities (i.e. shelters) separated from presumed COVID-19 negative individuals and staffed by health care professionals where individuals who are COVID positive can receive health care and assessments to see if they require higher level of care (i.e. transfer to emergency department or inpatient).
- Quarantine hotel/motel/trailers for those who could be safely isolated (e.g. those who are independent) and do not require extensive health care while contagious.
For people who are presumed to be COVID-19 negative:
- Hotels/motels/trailers for High Risk Persons, to prevent infection for individuals at high risk of medical complications.
- Shelters with appropriate social distancing.
- Remain unsheltered with appropriate outreach and social distancing.
For staff
- Staff should avoid switching between presumed COVID-19 negative work environments and persons under investigation/COVID-19 positive environments.
- OSHA recommends establishing alternating days or extra shifts that reduce the total number of employees working in shelter/quarantine/isolation space at a given time, allowing them to maintain distance from one another while maintaining a full work week onsite.
Sources:
- OSHA: Guidance on Preparing Workplaces for COVID-19
- UCSF Benioff Center: State of California Recommended Strategic Approaches for COVID-19 Response for Individuals Experiencing Homelessness
In ideal circumstances, what personal protective equipment should staff use?
PPE recommendations for people experiencing homelessness
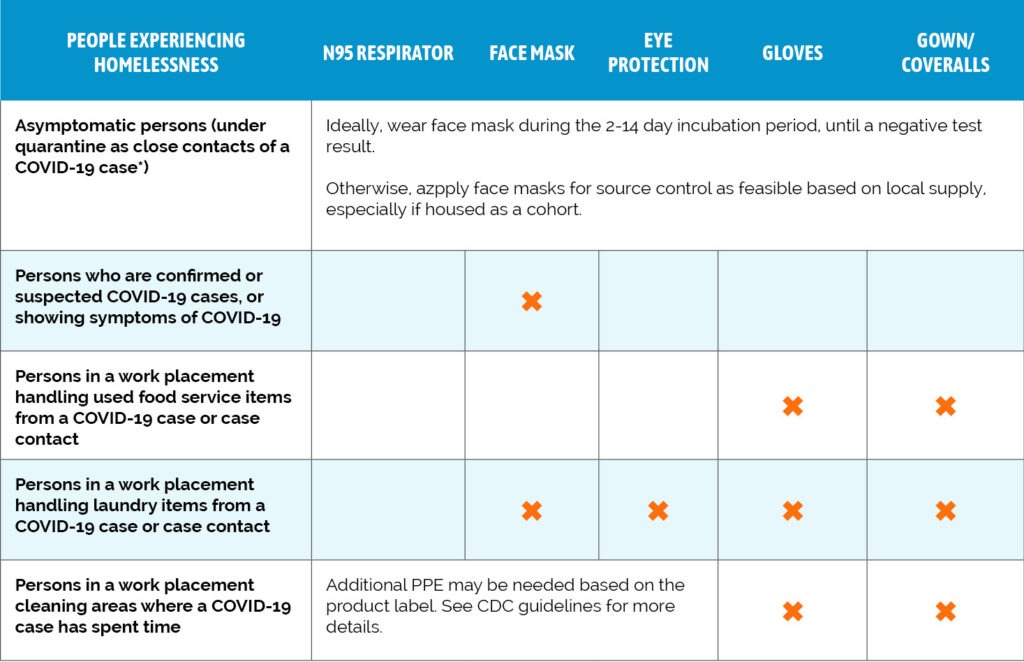
PPE recommendations for staff

Source
- CDC: Interim Guidance on Management of Coronavirus Disease 2019 (COVID-19) in Correctional and Detention Facilities
- While this was included in guidance for staffing in correctional facilities, we have confirmed with experts that these are the practices that are appropriate in any contexts where staff are working closely with people who may be COVID-19 positive.
How should staff use surgical masks?
Community Solutions has secured a supply chain to provide surgical face masks to Built for Zero communities in an effort to equip front line and other staff with elements of PPE (learn more here).
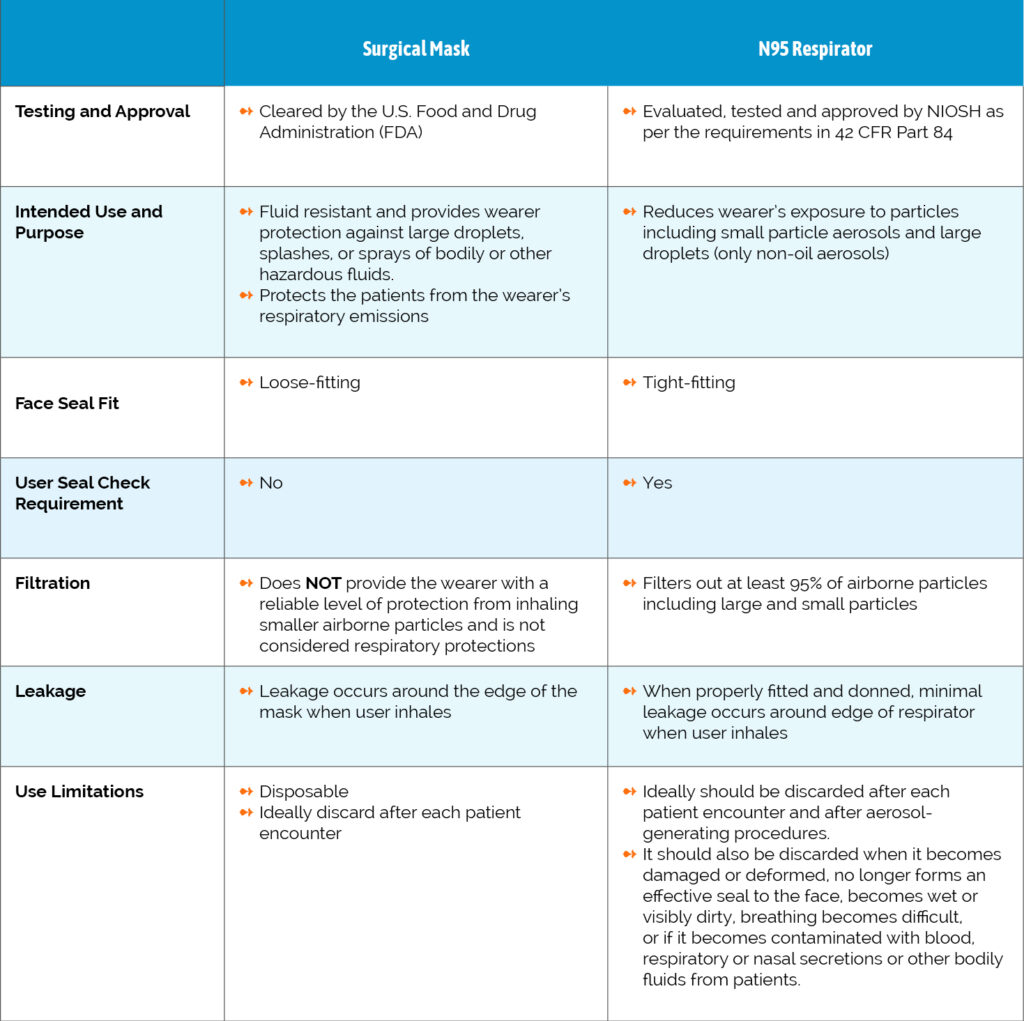
The FDA writes that “a surgical mask is a loose-fitting, disposable device that creates a physical barrier between the mouth and nose of the wearer and potential contaminants in the immediate environment. Surgical masks are regulated under 21 CFR 878.4040. Surgical masks are not to be shared and may be labeled as surgical, isolation, dental, or medical procedure masks. They may come with or without a face shield. These are often referred to as face masks, although not all face masks are regulated as surgical masks.
Surgical masks are made in different thicknesses and with different ability to protect you from contact with liquids. These properties may also affect how easily you can breathe through the face mask and how well the surgical mask protects you.
If worn properly, a surgical mask is meant to help block large-particle droplets, splashes, sprays, or splatter that may contain germs (viruses and bacteria), keeping it from reaching your mouth and nose. Surgical masks may also help reduce exposure of your saliva and respiratory secretions to others.
While a surgical mask may be effective in blocking splashes and large-particle droplets, a face mask, by design, does not filter or block very small particles in the air that may be transmitted by coughs, sneezes, or certain medical procedures. Surgical masks also do not provide complete protection from germs and other contaminants because of the loose fit between the surface of the face mask and your face.
Surgical masks are not intended to be used more than once. If your mask is damaged or soiled, or if breathing through the mask becomes difficult, you should remove the face mask, discard it safely, and replace it with a new one. To safely discard your mask, place it in a plastic bag and put it in the trash. Wash your hands after handling the used mask.”
A surgical mask differs from N95 Respirators in a few ways:
Sources
- FDA – Surgical Mask and Gown Conservation Strategies – Letter to Healthcare Providers
- CDC – Understanding the Difference
- FDA – N95 Respirators and Surgical Masks (Face Masks)
How should staff operate with a limited supply of personal protective equipment?
Maximize use of engineering controls, such as barriers and maintained ventilation systems, and administrative controls, such as altering work practices to minimize patient contacts.
Estimate your PPE needs, using the CDC’s PPE Burn Rate calculator.
Centralize control of PPE distribution.
Apply PPE contingency strategies immediately, rather than waiting until PPE is in short supply:
- Use reusable PPE that can be reprocessed wherever possible.
- For training, use PPE beyond the manufacturer-designated shelf life.
Consider extending use of respirators, facemasks, and eye protection beyond a single patient contact.
Consider crisis capacity strategies. Please note that the effectiveness of crisis strategies is uncertain and they may pose a risk for transmission between staff and patients.
- For interaction activities, consider using intact PPE that is beyond the manufacturer-designated shelf life.
- Carefully prioritize PPE use for selected care activities involving close contact.
- If no commercial PPE is available, consider following the CDC’s guidance on wearing cloth masks (details below).
Minimize chances for exposure.
- Restricting additional presence in areas with presumptively positive individuals as much as possible.
- Minimizing unnecessary face-to-face encounters.
Sources
- CDC: Strategies for Optimizing the Supply of Facemasks
- IHI: Recommendations for PPE Conservation: Restrict, Reduce, Re-Use
- CDC: PPE Burn Rate Calculator
- CDC: Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant Community-Based Transmission
Are cloth masks considered personal protective equipment?
- The CDC recommends that all people wear cloth face coverings in public settings where other social distancing measures are difficult to maintain, especially in areas of significant community-based transmission.
- However, homemade masks are not considered PPE, since their capability to protect health care providers is unknown. Caution should be exercised when considering this option.
- Homemade masks should ideally be used in combination with a face shield. Face shields provide full face coverage: they should cover the entire face, including mouth, nose, and eyes. They should cover the forehead, extend below the chin and wrap around the side of the face. The extended faceshield guidance is informed by the fact that it may be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their own mouth, nose, or possibly their eyes. This is not thought to be the main way the virus spreads, but the CDC and others are still learning more about this virus.
Sources
- CDC: Personal Protective Equipment (PPE) in Healthcare Settings
- CDC: Interim Guidance on Management of Coronavirus Disease 2019 (COVID-19) in Correctional and Detention Facilities
- CDC: Strategies to Optimize the Supply of PPE and Equipment
- CDC: PPE Burn Rate Calculator
- CDC: Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant Community-Based Transmission
- CDC: Strategies for Optimizing the Supply of Facemasks
- IHI: Recommendations for PPE Conservation: Restrict, Reduce, Re-Use
- CDC: How Covid-19 Spreads
What should staff do if there is a shortage of N95 respirators?
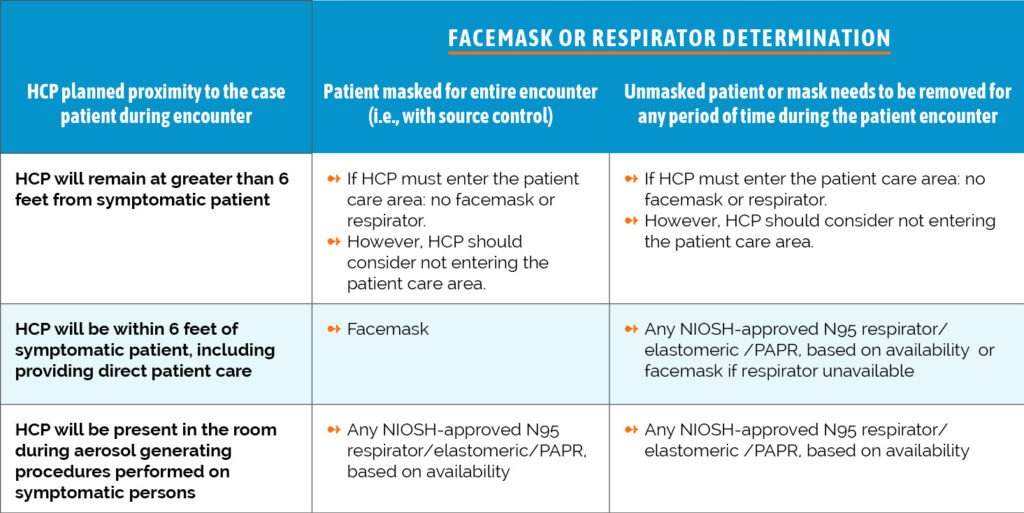
N95 or higher respirators are ideal for anyone in contact with presumed or confirmed COVID-19 positive individuals. The CDC recommends the following strategies for operating with a shortage of N95 respirators:
- Use of respirators beyond the manufacturer-designated shelf life
- Use of respirators approved under standards used in other countries that are similar to NIOSH-approved N95 respirators (list in link)
- Limited re-use of N95 respirators for COVID-19 patients
- Prioritize the use of N95 respirators and facemasks by activity type:
Source
What should staff do if there are no N95 masks?
- Exclude staff at higher risk for severe illness from COVID-19 from having contact with known or suspected COVID-19 patients;
- Designate convalescent staff for provision of care to known or suspected COVID-19 patients;
- As a last resort, use masks not approved by the National Institute for Occupational Safety and Health (NIOSH) or homemade masks, including cloth masks. In this case, use a face shield. Face shields provide full-face coverage: they should cover the entire face, including mouth, nose, and eyes. They should cover the forehead, extend below the chin, and wrap around the side of the face.
Sources
What should staff do if there is a shortage of facemasks?
- Exclude staff at higher risk for severe illness from COVID-19 from having contact with known or suspected COVID-19 patients.
- Designate convalescent staff for provision of care to known or suspected COVID-19 patients.
- As a last resort, use masks not approved by the National Institute for Occupational Safety and Health or homemade masks, including cloth masks. In this case, use a face shield. Face shields provide full face coverage: they should cover the entire face, including mouth, nose, and eyes. They should cover the forehead, extend below the chin, and wrap around the side of the face.
- Restrict facemasks to use by staff, rather than clients.
- Have clients follow the CDC’s guidance on wearing cloth masks.
Sources
Where can staff access training for putting on and taking off (donning and doffing) personal protective equipment?
Staff should be trained on the use of PPE and should be able to demonstrate competency in using PPE before interacting with clients. Appropriate donning and removing of PPE is critical to using it, and doing this incorrectly can dramatically reduce the protective impact of using PPE.
- The CDC has issued a generic training on the use of PPE.
- While written for a health care specific setting, these slides and trainer’s guidance can be used to train staff that will be working in isolation shelter and quarantine units and/or engaging in activities with clients listed in the table above.
Sources
- CDC: SLIDES – CDC Guidance for the Selection and Use of Personal Protective Equipment (PPE) in Healthcare Settings
- CDC: CDC-Issued Trainer’s Information (information to accompany training)
How should staff put on, or don, personal protective equipment?
More than one donning method may be acceptable. This is one example of donning.
- Identify and gather the proper PPE to don. Ensure choice of gown size is correct, based on training.
- Perform hand hygiene using hand sanitizer with alcohol.
- Put on isolation gown. Tie all of the ties on the gown. Assistance may be needed by other staff.
- Put on NIOSH-approved N95 filtering facepiece respirator or higher (use a facemask if a respirator is not available).
- If the respirator has a nosepiece, it should be fitted to the nose with both hands, not bent or tented.
- Do not pinch the nosepiece with one hand.
- Respirator/facemask should be extended under the chin.
- Both your mouth and nose should be protected.
- Do not wear a respirator/facemask under your chin or store in pockets between clients.*
- Respirator: Respirator straps should be placed on the crown of head (top strap) and base of neck (bottom strap).
- Perform a user seal check each time you put on the respirator.
- Facemask: Mask ties should be secured on the crown of head (top tie) and base of neck (bottom tie). If the mask has loops, hook them appropriately around your ears.
- Put on a face shield or goggles. Face shields provide full-face coverage. Goggles also provide excellent protection for eyes, but fogging is common.
- Before putting on gloves, perform hand hygiene.
- Gloves should cover the cuff (wrist) of gown.
- Staff may now enter client space.
Sources:
- CDC: Interim Guidance on Management of Coronavirus Disease 2019 (COVID-19) in Correctional and Detention Facilities
- CDC: Protecting Healthcare Personnel
- CDC: Using Personal Protective Equipment (PPE)
- CDC: Personal Protective Equipment FAQs
- CDC: Use Personal Protective Equipment (PPE) When Caring for Patients with Confirmed or Suspected COVID-19
- CDC: Guidance for the Selection and Use of Personal Protective Equipment (PPE) in Healthcare Settings
How should staff take off, or doff, personal protective equipment?
Three Reminders:
- PPE must be donned correctly before entering the area where there are persons under investigation and COVID-19-positive clients (e.g., isolation room, unit if cohorting).
- PPE must remain in place and be worn correctly for the duration of work in potentially contaminated areas. PPE should not be adjusted (e.g., retying gown, adjusting respirator/facemask) during patient care.
- PPE must be removed slowly and deliberately in a sequence that prevents self-contamination. A step-by-step process should be developed and used during training and patient care.
Doffing Method: More than one doffing method may be acceptable. Training and practice using your health care facility’s procedure is critical. This is one example of doffing.
- Remove gloves. Ensure glove removal does not cause additional contamination of hands. Gloves can be removed using more than one technique (e.g., glove-in-glove or beaking method).
- Remove the gown. Untie all ties (or unsnap all buttons).
- Health care personnel may now exit the room.
- Perform hand hygiene.
- Remove face shield or goggles.
- Carefully remove face shield or goggles by grabbing the strap and pulling upwards and away from head.
- Do not touch the front of the face shield or goggles.
- Remove and discard respirator (or facemask if used instead of respirator). Do not touch the front of the respirator or facemask.*
- Respirator: Remove the bottom strap by touching only the strap and bring it carefully over the head. Grasp the top strap and bring it carefully over the head, and then pull the respirator away from the face without touching the front of the respirator.
- Facemask: Carefully untie (or unhook from the ears) and pull away from face without touching the front.
- Perform hand hygiene after removing the respirator/facemask and before putting it on again if your workplace is practicing reuse.*see note
Note
* Facilities implementing reuse or extended use of PPE will need to adjust their donning and doffing procedures to accommodate those practices.
Please see this CDC webpage for additional information on donning and removing PPE. And, if you have questions on use of any particular PPE (gowns, gloves, respirators), the CDC has created an FAQ page.
Sources
- CDC: Interim Guidance on Management of Coronavirus Disease 2019 (COVID-19) in Correctional and Detention Facilities
- CDC: Protecting Healthcare Personnel
- CDC: Using Personal Protective Equipment (PPE)
- CDC: Personal Protective Equipment FAQs
- CDC: Use Personal Protective Equipment (PPE) When Caring for Patients with Confirmed or Suspected COVID-19
- CDC: Guidance for the Selection and Use of Personal Protective Equipment (PPE) in Healthcare Settings
How should staff use gloves?
Use gloves whenever possible. If you do not have gloves, avoid touching your face without having previously washed your hands.
Gloves are not a substitute for hand hygiene. If you are using gloves, please wash your hands in accordance with CDC guidelines before donning and after removing gloves.
Sources
- CDC: Interim Guidance on Management of Coronavirus Disease 2019 (COVID-19) in Correctional and Detention Facilities
- CDC: Strategies to Optimize the Supply of PPE and Equipment
- CDC: Hand Hygiene in Healthcare Settings
How should staff clean high-touch spaces in my space?
Where can staff go to try to secure more personal protective equipment?
Contact the FDA. The FDA has issued a letter to health care providers that summarizes the aforementioned CDC guidance for conserving surgical masks and gowns in the face of limited supply. In this letter, the FDA has requested that anyone facing potential or actual supply issues should email information to the FDA at deviceshortages@fda.hhs.gov.
Utilize the following resources:
- Project N95 is a national clearinghouse to connect health care providers with critical equipment.
- PN95 is coordinating with manufacturers and suppliers to secure personal protective equipment to front-line medical workers across America.
- Although the website notes that it is for health care providers, New America confirmed that homeless service providers can also apply.
- Project C.U.R.E. is also working to connect local government agencies, health care operations and Emergency Medical Service Providers in the United States with PPE.
- Although the website notes that it is for health care providers, a representative from Project C.U.R.E confirmed that homeless service providers can also apply.
- Please use this form to make requests
- Battelle, a global research and development organization committed to science and technology for the greater good, was approved by the FDA as a Critical Care Decontamination System (CCDS). This CCDS can decontaminate N95 respirators for reuse. The process for sending in used respirators to be cleaned and returned is detailed here.
- Community Solutions reached out to Battelle to see if nonprofits and government agencies in the homelessness response system were able to use this cleaning service. As of April 9, 2020, we have not yet received confirmation.
Sources
- FDA: Surgical Mask and Gown Conservation Strategies – Letter to Healthcare Providers
- Project N95
- Project C.U.R.E.
- Battelle
QUALITY CHECK
Learn more about our process for vetting information.


